Introduction
Background
Aspiration, ie, the act of taking foreign material into the lungs, can cause a number of syndromes determined by the quantity and nature of the aspirated material, the frequency of aspiration, and the host factors that predispose the patient to aspiration and modify the response. Three types of material cause 3 different pneumonic syndromes. Aspiration of gastric acid causes chemical pneumonia (CP). Aspiration of bacteria from oral and pharyngeal areas causes bacterial pneumonia (BP). Aspiration of oil, eg, mineral oil or vegetable oil, causes exogenous lipoid pneumonia, a rare form of pneumonia. In addition, aspiration of a foreign body may cause an acute respiratory emergency and, in some cases, may predispose the patient to bacterial pneumonia.
Aspiration pneumonia, according to common usage, includes both CP and BP, although the pathophysiology, clinical presentation, treatment, and complications of CP and BP are different.
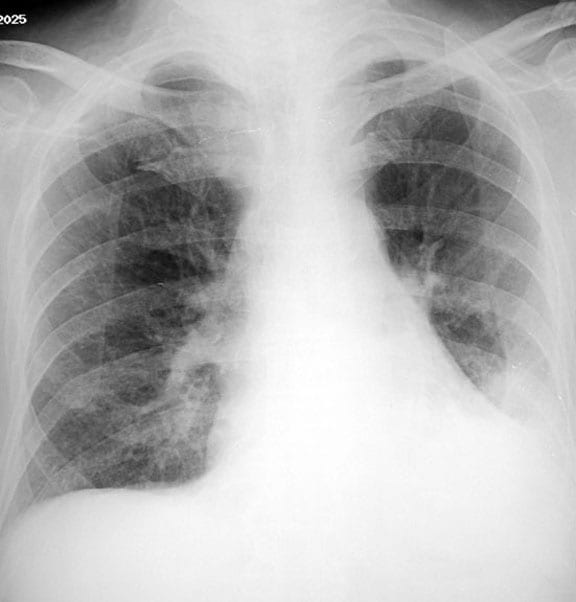
Note the image below.
Aspiration pneumonia. An 84-year-old man in generally good health had fever and cough. Posteroanterior radiograph demonstrates a left lower lobe opacity.
Pathophysiology
Aspiration of small amounts of material from the buccal cavity, particularly during sleep, is not an uncommon event. No disease ensues in healthy persons because the aspirated material is cleared by mucociliary action and alveolar macrophages. The nature of the aspirated material, volume of the aspirated material, and state of the host defenses are 3 important determinants of aspiration pneumonia.
CP, also known as Mendelson syndrome, is due to the parenchymal inflammatory reaction caused by a large volume of gastric contents independent of infection. If the pH of the aspirated fluid is less than 2.5 and the volume of aspirate is greater than 0.3 mL/kg of body weight (20-25 mL in adults), it has a greater potential for causing CP. The initial chemical burn is followed by an inflammatory cellular reaction fueled by the release of potent cytokines, particularly tumor necrosis factor–alpha and interleukin-8.
BP caused by aspiration can occur in the community or in the hospital (ie, nosocomial). In both situations, anaerobic organisms alone or in combination with aerobic and/or microaerophilic organisms play a role. In anaerobic pneumonia, the pathogenesis is related to the large volume of aspirated anaerobes (eg, as in persons with periodontal disease) and to host factors (eg, as in alcoholism) that suppress cough, mucociliary clearance, and phagocytic efficiency.
Nosocomial BP caused by aspiration is common, and the major pathogens involved are hospital-acquired florae through oropharyngeal colonization (eg, enteric gram-negative bacteria, staphylococci). Selection and colonization of gram-negative organisms in the oropharynx, sedation, and intubation of the patient's airways are important pathogenetic factors in nosocomial pneumonia.
Frequency
United States
A reliable estimate of incidence of CP is not available. BP caused by aspiration is reported to cause 5-15% of community-acquired pneumonia (CAP) cases. Nosocomial BP is the second most likely cause of nosocomial infections, second only to urinary tract infection, and is the leading cause of death from hospital-acquired infections.
Mortality/Morbidity
In Mendelson's original series in 1946, Mendelson described 61 obstetric patients who aspirated gastric acid during anesthesia, all of whom had a complete clinical recovery within 24-36 hours.1 In subsequent studies, which have included older sicker patients, CP has a reported mortality rate of 30-62% because CP often leads to acute respiratory distress syndrome (ARDS).
If BP is not treated early, it can lead to development of complications, including lung abscess and bronchopleural fistula.
Nosocomial pneumonia is associated with a longer period of hospitalization and increased mortality rates.
Age
Nosocomial BP caused by aspiration is much more frequent in adults than in children. Predisposing factors (see Causes) are more common among elderly people; therefore, this population is more prone to develop aspiration pneumonia. Comparative studies of BP in patients from the community with those in a continuing care facility have shown a 3-fold increase in the latter population (the majority of them had neurologic disease with dysphagia).2
Clinical
History
Chemical pneumonitis findings are as follows:
- Acute onset
- Abrupt development of symptoms within a few minutes to 2 hours of the aspiration event
- Respiratory distress and rapid breathing
- Audible wheezing
- Cough with pink or frothy sputum
Bacterial pneumonia findings are as follows:
- Community acquired
- Subacute or insidious onset: Symptoms manifest in days to weeks when anaerobic organisms are the pathogens.
- Cough with purulent sputum
- Absence of rigors
- Putrid odor of sputum (a clue to anaerobic bacterial pneumonia)
- Weight loss
- Hospital acquired: Symptoms of cough and shortness of breath of may be more acute in onset than in CAP when aerobic organisms are the pathogens; fever and rigors may be present.
Physical
Chemical pneumonia findings are as follows:
- Tachypnea
- Tachycardia
- Fever
- Rales
- Wheezing
- Cyanosis (possibly)
Bacterial pneumonia findings are as follows:
- Community acquired with anaerobic etiology
- Periodontal disease (primarily noted as gingivitis)
- Bad breath
- Clubbing of fingers (possibly)
- Hospital acquired
- Fever
- Bronchial breath sounds and rales over a consolidated posterior area
Causes
Almost all patients who develop aspiration pneumonia have one or more of the predisposing conditions listed below. While all the listed conditions predispose the patient to chemical pneumonia (CP), conditions that alter consciousness and periodontal disease specifically predispose the patient to bacterial pneumonia (BP).Conditions associated with altered or reduced consciousness are as follows:
- Alcoholism
- Drug overdose
- Seizures
- Stroke
- Head trauma
- General anesthesia
Esophageal conditions are as follows:
- Dysphagia: Orophayngeal dysphagia has been found in the majority of elderly patients (mean age, 84 y).3
- Esophageal strictures
- Esophageal neoplasm
- Esophageal diverticula
- Tracheoesophageal fistula
- Gastroesophageal reflux disease
Neurologic disorders are as follows:
- Multiple sclerosis
- Dementia
- Parkinson disease
- Myasthenia gravis
- Pseudobulbar palsy
Mechanical conditions are as follows:
- Nasogastric tube
- Endotracheal intubation
- Tracheostomy
- Upper gastrointestinal endoscopy
- Bronchoscopy
- Gastrostomy or postpyloric feeding tubes
Other types of conditions are as follows:
- Protracted vomiting
- Prolonged recumbency
- General deconditioning and debility
- Critical illness

No comments:
Post a Comment